Sometimes, negative emotions are not directly related to blood sugar, but more indirectly related to diabetes: people may be dissatisfied with their self-management, feel frustrated/guilty about high/low blood sugar, experience a lack of understanding in people around them. And of course: having diabetes is no fun. Having negative emotions about diabetes every now and then, is a normal and healthy response.
However, when emotions about diabetes are too negative, it is good to acknowledge that, and to try to take some action.
If you want to learn more about negative emotions related to diabetes, we have more information for you. In the menu item “Managing your Emotions” you will find various texts on specific negative emotions related to diabetes, such as low mood/depression, feeling anxious about hypo’s, feeling anxious about complications, feeling stressed or tired, feeling burned out by your diabetes. Just take a look in our ‘’online library’’ and learn more about negative emotions in diabetes.
Author: Manuela Plössnig
Coping with negative emotions because of exercise
We know that many people with diabetes experience negative emotions because of their diabetes. These negative emotions can be any negative emotion, such as anxiety, anger, shame, guilt, failure.
Sometimes these negative emotions are directly related to a specific part of diabetes self-management. Of course, no part of diabetes self-management is really ‘’fun’’ or enjoyable. But some activities might induce more negative emotions than others. You mentioned, that doing exercise gives you negative emotions. This is important to know. We hope we can help you modify those feelings.
- Do you know which negative emotion you have about exercise? Does it feel boring? Do you feel sad about it? Do you feel angry, that you have to spend time on it? Are you anxious about having hypo’s? Or maybe too self-conscious about your looks while doing sports?
Or maybe there is another negative emotion that you are aware of. - It is important to realize that emotions always are ‘’true’’, these are your individual feelings. They might not be useful, or logical, but that is the way you feel. In the section “Managing your Emotions” you will find specific information about specific emotions, such as feeling anxious about hypo’s, feeling stressed, feeling depressed/sad. If you recognize any of these emotions, please take a look at the website to read the texts that refer to what you are feeling
- Another thing to ask yourself is: do you feel ‘’good’’ ‘’better’’ or positive in any way, AFTER sports/exercising? If so, you are probably still on the right track…, but your brain might just need more time to ‘’get used to’’ this new behaviour. The positive feeling afterwards works as an important reward for your brain, but it takes time for your brain to ‘’connect’’ this positive feeling (reward) to sports/exercise. If you would continue to perform your exercise/sports, and you would have this positive feeling afterwords, your brain will even learn to long for this feeling …, and make you want to perform sports/exercise more and more…
If you have tried to do sports/exercise for a while, and you keep experiencing negative emotions without the ‘’reward feeling’’ afterwards, then it may be time to adjust your goal. Click here if you want to read more on why and how to adjust a goal. Click here if you want to read more on how chose different ‘’exercise’’ goals.
Adjusting goals
When you are not making progress in your goal(s), it is good to reflect on what is happening. In most cases, lack of goal progress is only temporary and situational: the circumstances in the past week(s) probably were different from what you had anticipated on. Maybe you got the flu/a cold, maybe you were busy at work, maybe your family needed special care… These are no things to worry about, and they will probably not last for a very long time. They will not prevent you from reaching your goal, eventually.
However, when you feel your lack of goal progress is not so temporary, it might be good to revise and adjust your goals. Pursuing unrealistic or even impossible goals is not only frustrating, but even influences our mood, self-esteem and self-efficacy in the long term. Our brain stores all negative experiences with this goal and creates a ‘’negative network’’ in our brain. This ‘’negative network’’ makes us feel negative about this goal and behaviour, and harms our self-efficacy and mood. As a consequence we might even feel resistance towards this goal.
Of course, that is not helpful in any way!
In order to change behaviour effectively, we have to create ‘’positive experiences’’ with the new behaviour. Our brain needs to develop a ‘’positive network’’ about the new behaviour. A network that makes us feel good about ourselves, and influences our mood and self-esteem positively.
That is why it is better to achieve smaller and more realistic goals, than to keep trying (and fail) to achieve bigger, unrealistic goals.
If you think you might benefit from goal adjustment: take some time to reformulate your goal. Usually this does not mean that you will completely have to leave the goal…., it is just a matter of taking a step back. For instance: when your goal was to check your blood sugar with every meal, but you find yourself ‘failing’ every day, it is much better to just pick one meal that you would like to focus on. Pick the most realistic one. So, if you know that checking your blood sugar before breakfast is easier to achieve than during lunch at work, start with the goal to check your blood sugar every morning at breakfast. That is an important and helpful first step in optimizing your blood sugar!
When you realize that you have been able to achieve this goal for some time, congratulate yourself! Your brain has started to create a ‘’positive network’’ on this behaviour. That will help you in taking the next step.
Successful behaviour change is also about being happy with every small change that you are able to realize, and not putting yourself down for all the things you have not achieved yet.
Good luck!!
About negative emotions because of your diabetes
We know that many people with diabetes experience negative emotions because of their diabetes. These negative emotions can be any negative emotion, such as anxiety, anger, shame, guilt, failure.
Sometimes these negative emotions are directly related to high or low blood sugar. When having high or low blood sugar, many people experience negative emotions. Research even shows a relationship between higher HbA1c’s and negative emotions.
Many negative emotions, in various diabetes related situations can arise.
You mentioned, that monitoring your glucose gives you negative emotions.
Try to ask yourself: is my negative emotion a direct consequence of my low/high blood sugar? (‘’Do I feel physically uncomfortable, and therefore emotionally negative?’’)
Or is my negative emotion a more indirect consequence of my diabetes (such as feelings of disappointment or failure)?
If your negative emotion is DIRECTLY the consequence of high/low blood sugar, the best thing you can do is focus on optimizing your blood sugar, and not on the emotions. When experiencing high or low blood sugarsour brain is negatively influenced and more vulnerable to negative emotions. We just cannot prevent them… The only thing we can do is try to prevent the higher and lower blood sugar (and we will not always succeed…L), and tell the people who are close to us, that these negative emotions are part of dealing with diabetes…. This is no fun, but it is good to be realistic about these negative emotions, and to understand that they are just temporary. As soon as our blood sugar stabilize, our emotions will stabilize as well.
Click here if you want to learn more about emotions that are more Indirectly related to diabetes. Or, if you want to do it later, schedule an [activity
Coping with your fear of hypoglycaemia
You may have used the tips and advices we gave when you recognized your fear of hypoglycaemia and your excessive safety behaviours.
In case you forgot them, you can click on this link, to Worrying about low blood sugar.
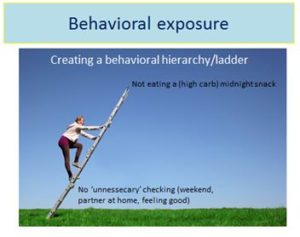
If you want to work on limiting the excessive safety behaviours yourself, you could make a so called ‘’safety ladder’’. By means of this ladder you will be able to make a hierarchy of your fears and safety behaviour, and to take a first step in changing your behaviour.
Before trying to make this ladder and changing your behaviour, it is good to think about the purpose of trying. Why would you change your behaviour? And what will it do for you?
One of the reasons of changing your safety behaviours is that we hope you will be able to broaden your comfort zone.
When you take a look at this picture, you can see your comfort zone in green. This is the ‘so called zone’ that you feel comfortable in. With your safety behaviours you will make yourself feel safe and as comfortable as possible. However, this means that you ‘offer’ some freedom and flexibility. The more safety behaviours you perform, the more safe you will feel. But the more anxious you will feel when you are outside of your comfort zone.
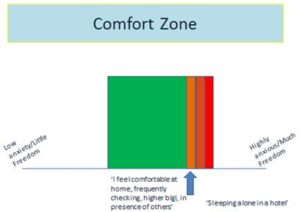
In the picture you see an example of someone who feels comfortable in his comfort zone performing his personal safety behaviours: staying at home, frequently checking blood glucose, or always being in the presence of others.
When this person is not able to perform (all) his safety behaviours he will need to step outside of his comfort zone. Which, of course, feels anxious and uncomfortable. And the more he stays in his comfort zone, the less comfortable he feels when having to step outside his comfort zone.
In the example you see ‘’sleeping alone in a hotel’’. That would be described as his worst nightmare: not having others around, and going to bed alone would be the most frightening thing he could imagine.
You’ll probably understand that his anxiety would be extreme, when he would be forced to do this. And he would probably quickly return to his comfort zone, to never step out of it again J
When trying to reduce anxiety it is important that you will try to do it slowly and stepwise.
That is what the ‘’safety behaviours ladder’’ is for!
Below, you find an example of such a ladder. For this person, not eating a midnight snack (and thus having ‘’lower’’ blood sugar in the night) would be the most frightening thing to do. That would not be a very wise first step.
However, this person thought of a first step: ‘’Not unnecessarily checking blood glucose when feeling ok and relaxed, and his partner being around…’’ That step would make him only feel slightly uncomfortable, but would certainly not be his worst case scenario.
This would be something he could start to practice. First telling his partner about it (for emotional support and help!), and then starting to ‘’not measure blood glucose’’ under these specific conditions.
Question: try to think of a first step on your ‘’safety behaviour ladder’’.
Which safety behaviour would you be able to let go of, under specific conditions, and only feeling slightly uncomfortable?
Would it be one less measurement of glucose? Not eating a carb snack? Injecting a little more insulin? Going out/doing physical exercise?
Write down the specific behaviour, and discuss it with at least one person. Try to perform the behaviour a few times.
Worrying about low blood sugars
Many people with diabetes worry about having low blood sugar (hypoglycaemia, or ‘hypo’s’).
To a certain extent, worrying about low blood sugar is a normal and healthy phenomenon in all diabetes patients on insulin (or other blood glucose lowering medication). However, in some people normal and healthy worries develop into hindering anxieties, that influence their blood sugars and quality of life. Often, these anxieties develop after having experienced a serious hypo, needing help from others, and/or being unconscious. But in some people these hindering anxieties might also develop without having experienced a serious hypo.
Many people with fear of hypoglycaemia worry about:
-having a hypo while asleep (or even dying from a hypo in their sleep)
-losing consciousness in public, while driving or being alone at home
-needing help from others, attracting unwanted attention
In some people these anxieties are so intense that they will make sure their blood sugar never drop below a certain level. They might eat some extra carbs before going to bed, before/while driving, or before going out, even when their blood sugar don’t really ‘need’ an extra snack. Or otherwise, people might use less insulin than they should, just to make sure that their blood sugar won’t drop. Some might check their blood sugars excessively, to monitor potential blood sugar drops.
These are all common behavioural reactions to anxiety, and are called ‘’safety behaviours’’. In the short term, these safety behaviours help to prevent/decrease anxiety. However, in the long term, these behaviours make people more insecure about low blood sugar, and help to develop even more anxiety.
That is why it is so important to limit the ‘’safety behaviours’’ to a healthy and rational amount.
If you recognize these anxieties and safety behaviours, there are a few steps to take:
- it is good to let others know about it. Best would be to inform your partner/significant other, as well as your diabetes health care professional (s).
- make a list of the questions/worries you have about hypo’s. Explain what your fears are about
- make a list of the specific safety behaviours that you perform to reduce your anxiety
- let a diabetes health care professional educate you about hypoglycaemia
- let a diabetes health care professional help you in making a stepwise plan on how to limit these safety behaviours
Importance of Exercise
In general, exercise is a wise thing to do: having diabetes or not. But for people with diabetes, exercise (or being physically active) is even more important. Just like nutrition, exercise helps to regulate blood glucose. Even to that extent that people who do not use diabetes medication yet, can prevent starting diabetes medication by exercising regularly (in combination with healthy eating). For people who (already) use diabetes medication, exercising helps to make the body more sensitive to insulin. That is why many people who use diabetes medication and perform exercise, experience that they need less medication when they are more active. This advantage does not only occur DURING exercise, but even several hours after. Depending on the type and duration of your exercise, you might benefit from increased insulin sensitivity even a day after your exercise. That means that people with diabetes who exercise regularly (at least 3 times a week) can even lower their general need for diabetes medication. And increased insulin sensitivity and less diabetes medication often also means: better circumstances to lose weight. Low insulin sensitivity makes it more difficult to lose weight.
And of course: all general advantages of being physically active still hold: feeling more energetic and positive, increased resilience to stress, and significantly lower risks of cardiovascular
Why exercises are important
Our brain has less attention for things that are not important to us, so it is hard to perform a behaviour with less attention.
In general, we can say that doing sports, performing exercise is healthy for EVERYONE, and especially for people with diabetes. But, of course, it will depend on personal preferences and health conditions what type of activities, which intensity and duration are beneficial.
Many people who have always felt uncomfortable or even negative about sports, have difficulty becoming more active.
It is good to understand that ‘’being more active’’ has many definitions. Research on health benefits of ‘’exercise’’ has shown that simple activities, that are not really associated with sports/exercise can even have the same positive influence on health outcomes as real sports/exercise.
Research even shows the positive influence of ‘’standing’’ versus ‘’sitting’’. Even without really moving, we can increase our health by just simply standing more. So ‘’being more active’’ could also simply imply: sitting down less… Try to be creative in thinking of activities that you could perform standing instead of sitting: e.g. reading the newspaper, watching television, making a telephone call.
If you could replace one sitting behaviour by a standing behaviour every day, you can consider yourself successful in a first step to better health. Just start here, and try to come up with more of such small behaviour changes regarding standing, increased activity without necessarily thinking of sports/exercise.
How to deal with frustration
Sometimes, people with diabetes try their hardest without any apparent result… They injected insulin/took their medication, they monitored glucose, they watched their foods, they exercised, and still their blood sugar values are not in control… Of course, this might lead to feelings of frustration or even thoughts such as ‘’Why am I doing all this?’’ ‘’Does this have any effect, at all?’’
We can totally understand these thoughts and feelings. And they are perfectly normal.
However, we can tell you that your effort in self-management is ALWAYS useful! Always.
Unfortunately, diabetes is no mathematics. It might be tempting to think in mathematical terms, but in the world of diabetes maths means that 2+2 = 4, but sometimes it is 6, or even 7 or 2.5. Without any clear reason.
Most people with diabetes find that extremely frustrating. You are trying so hard, and yet: it seems as if nothing happens..
Keep in mind that if you would do NOTHING or LESS it would be much worse. That means your effort in self-management makes a change!!! It is just not visible how your effort helps in preventing this worse situation. That is important to remember: your intentions were the best, but it just did not work out the way you hoped…. The next time it probably will.
At these moments it is good to keep in mind that diabetes is no mathematics, and that you can only do your best. Try not to be too negative about your actions/y
Forgetting about diabetes self-management
In daily practice, many people with diabetes say that they ‘forget’ about specific parts of diabetes self-management. They forget to monitor glucose, or forget to inject insulin before meals, or forget to take their tablets, or forget to count carbs or to exercise. It is not that they are not motivated, or that they don’t want to take care of themselves, but it is just no automatic response (yet). That is understandable! Diabetes is a complex disease with many things to do, so it is logical that people forget about some things every now and then. Don’t worry. These occasional ‘missings’ don’t influence your average glucose values (HbA1c) a lot.
However, when the ‘missings’ are not occasional, but more regular, you might think about why this happens and how to solve it. The first thing to ask yourself is whether you really ‘’did not think of doing it at all’’. E.g. have you really NOT thought about injecting your insulin, monitoring your glucose etc? No? That is the easy-to-change-part!
You could:
- Create a (n extra) cue to make sure you won’t forget the plan: make a reminder in your phone/computer, put a note/post-it on a place that you see most of the day
- Make sure that your plan is explained/mentioned to at least one person who is close to you. He/she could simply ask how you are doing, and whether your plan worked out.
However, many people do think injecting insulin, monitoring glucose etc. for a second, but then immediately afterwards, think: ‘’I will first finish…..[whatever you are doing] and then inject my insulin/monitor my glucose etc. a little later…’’ Technically speaking, this is NOT really a matter of forgetting, but more of postponing. You WERE thinking about it for a second/minute, but did not want to/could not stop the other activity you were performing.
That is something you could (gradually) change. You are not really forgetting to self-manage, but you will have to try to postpone less, or do it immediately when you think about it.
Practice with : ‘’postponing less’’ first, in stead of ‘’’not forgetting’’ or ‘’doing it immediately’’. For instance: if you sometimes only would inject insulin an hour after your dinner, try to practice with ‘’injecting earlier after dinner’’ in stead of doing it immediately at the dinner table. You are successful in behaviour change, with every minute that you postpone less. You might e.g. create a cue around the dishwasher, so that you are reminded of ‘’postponing less’’ shortly after dinner. This reduce in time can make a significant contribution to optimizing your blood sugar.